
Closed-angle (or pupillary-block) glaucoma/ narrow angle glaucoma are some of many types of glaucoma. Laser Iridotomy is used to treat closed-angle glaucoma or prevent closed-angle glaucoma in those who have narrow angle glaucoma. During a laser iridotomy, a very focused beam of light is used to create a hole on the outer edge of the iris, the colored part of the eye. This opening allows fluid (aqueous humor) to flow between the anterior chamber, the front part of the eye, and the area behind the iris, the posterior chamber. This opening may decrease the pressure in the eye and usually prevents sudden build up of pressure within the eye, which occurs during an episode of acute closed-angle glaucoma.
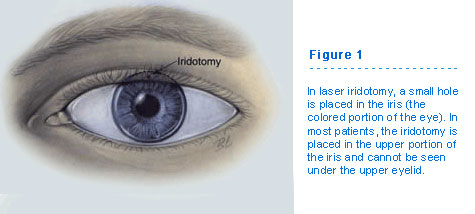
To better understand closed-angle glaucoma and its treatment, iridotomy (Figure 1), it is important to understand the different factors which determine eye pressure.
What is Eye Pressure?
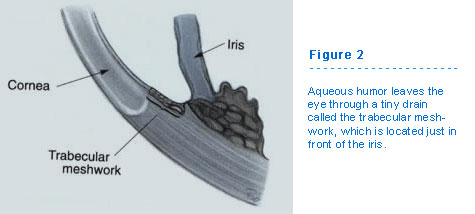
Your eye is partly filled with a nourishing fluid, called the aqueous humor. It is made just behind the iris. The aqueous fluid then flows forward, pass the iris and lens, and into the front chamber of the eye where the eye’s drainage system, the trabecular meshwork (figure 2, 3a), is located. From the drain, it flows into the blood stream. (It has nothing to do with tears; tears cover the front surface of the eye only.)
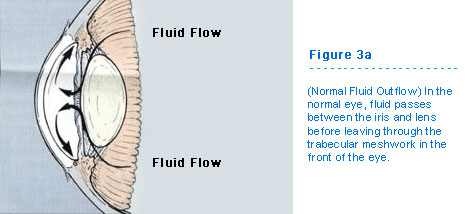
The balance between how much fluid is made, and how much leaves the eye, determines the pressure within the eye. All eyes have measurable pressure. However, when the amount of aqueous humor draining from the eye is reduced, the pressure within the eye can increase. This high pressure often leads to glaucoma.
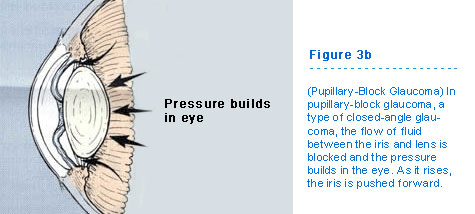
Although many people think of glaucoma as just one single disease, in fact there are many different forms of glaucoma. Differences depend upon where in the eye the blockage to the drainage occurs. Both the border between the iris and lens as well as the trabecular meshwork are areas where the flow of aqueous fluid can be limited, leading to increased eye pressure. One type of glaucoma, pupillary-block glaucoma, occurs with the former. In this type of closed-angle glaucoma, the flow of fluid between the iris and lens is blocked (Figure 3b). It is called pupillary-block glaucoma because the fluid is trapped behind the pupil.
Pupillary-Block Glaucoma
As many as 10% of all glaucoma patients in the United States may have pupillary-block glaucoma. The blockage of fluid flow between the iris and lens can cause the pressure behind the iris to rise. As it rises, the iris is pushed forward. If it moves forward enough, the iris can cover the trabecular meshwork like a rubber stopper in a drain.
Sometimes a patient is unaware of the pupillary-block. However, the eye may become red. A patient also may experience headache or pain, blurred vision, and halos around lights. Rarely, there is nausea.
If there is sudden pupillary-block and if the eye is left untreated, permanent damage can occur which can lead to blindness.
The sooner the blockade of fluid flow between the border of the iris and lens is treated, the less damage occurs. Therefore, it is desirable to treat this disease as early as possible.
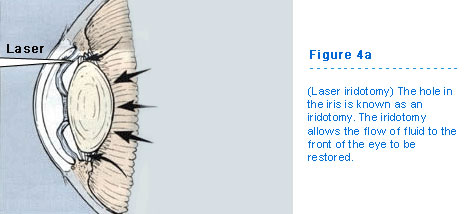
The best treatment for pupillary-block glaucoma is to create a hole in the iris, an iridotomy. (Figure 4A). The iridotomy allows the flow of fluid to the front of the eye to be restored, bypassing the pupil, the location of the blockade (Figure 4B).
The term “narrow angle glaucoma” simply means that you are at a higher risk of developing closed-angle glaucoma. Patients with Narrow Angle Glaucoma should avoid medications such as cold remedies which contain Pseudoephedrine, Phenylephrine or Neo-Synephrine, anti-histamines such as Chlorpheniramine, Diphenhydramine or Benadryl, and overactive bladder remedies such as Detrol. These remedies along with other medications not mentioned above often carry a warning telling you not to use them if you have glaucoma. If your Narrow Angle Glaucoma has been treated with laser, these medicines become safe for you to use.
How do lasers work to treat glaucoma?
Lasers deliver a type of light energy. This type of light energy is similar to using a magnifying glass to harness the energy of the sun to burn a hole in a piece of paper on a sunny day. The magnifying glass needs to properly focus the light to create a hole in the paper. Likewise, if the laser is not aimed properly at the iris, there is no effect. In order to focus the laser, your eye doctor uses an instrument called a slit-lamp.
This is the same instrument which is used to routinely examine your eyes. Since this is actually a type of microscope, the laser energy can be focused with extreme accuracy.
Several types of lasers can be used to treat pupillary-block glaucoma. The use of the argon laser to create an iridotomy was accepted widely by 1980. Since then, another type of laser, the neodymium:YAG laser, also has proven to be safe and effective. Although there are some differences between these two types of lasers, the use of one or another is best left to your ophthalmologist.
How is laser iridotomy performed?
Before having an iridotomy, your ophthalmologist may place some different types of drops on your eye. The first drop, pilocarpine, will make your pupil smaller. This stretches and thins your iris, similar to stretching out the top surface of a drum. By doing this, it is easier for the laser to penetrate and make a hole in your iris. You may be asked to continue using this eye drop for a few days following the laser treatment. This medication may temporarily cause blurred vision (especially at night) and also may give you a brow-ache.
Another type of eye drop may be used within a few hours of your laser treatment to prevent eye pressure from increasing following laser treatment, or to treat eye pressure that already has increased. Still other eye drops may be used to reduce inflammation.
The only kind of anesthesia required to perform a laser iridotomy is an eye drop (Figure 5). This is the same type of drop which your doctor places in your eye when the eye pressure is measured. With the eye drop, the laser surgery should be painless. You may see a bright light, like a photographer's flash from a close distance. Also, you may feel a pinch-like sensation.
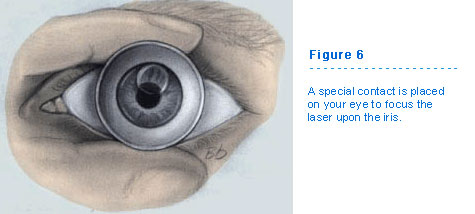
Your doctor will next place a special contact lens on your eye to focus the laser light upon the iris (Figure 6). This lens keeps your eyelids separated so that you do not blink during the treatment. This also reduces small eye movements so that you do not have to worry about your eye moving during the treatment. To protect the eye from being scratched by the contact lens, special jelly is placed on its surface. This jelly may remain on your eye for about 30 minutes, leading to blurred vision or a feeling of heaviness. The treatment is usually performed one eye at a time and is usually required in both eyes. Closed-angle glaucoma usually affects both eyes over time. Once sudden(acute) closed-angle glaucoma occurs in one eye and laser treatment has been done on that eye, laser iridotomy is usually done on the other eye to prevent the condition from developing in the other eye. Without treatment, there is a 50% chance that closed-angle glaucoma will also develop in the unaffected eye.
What to expect after an iridotomy.
After treatment, your doctor may ask you to stay for a few hours to check your eye pressure and insure that it has not increased.
When it is safe, you will be sent home and may be asked to use eye drops. Your ophthalmologist will explain their use and when you need to be examined again.
In general, there are no restrictions in activity following the laser treatment. You can return to your normal daily chores immediately. It is advisable to have someone drive you home from your doctor's office. You can expect some redness of the eye, a sensitivity to light, and a scratchy sensation. All of these might last for a period of days. You also might expect a small headache later that day or night.
You may notice a line of glare or a “hair” in your field of vision occasionally for a few weeks after treatment. This occurs because light may enter the laser opening, like passing through a second pupil. It occurs more commonly in bright lights, like sunlight, or when you move your eye and/or open the eyelids widely. Do not worry. This means a successful opening is present, and therefore, in general, is a good sign. This sense of glare, which may be slightly annoying at first, will fade over time as your brain adjusts to having the spot present.
PRE/POST OP INSTRUCTIONS (link)
The chance of losing vision following a laser procedure is extremely small. The main risks of a laser iridotomy are that your iris might be difficult to penetrate, requiring more than one treatment session. The other risk is that the hole in your iris will close. This happens less than one-third of the time. Once the hole stays open for six weeks, it is unlikely that it will close in the future. In addition, you may still require medications, or other treatments to keep your eye pressure sufficiently low. This further treatment is necessary if there is damage to the trabecular meshwork prior to the iridotomy or if you also have one of the other types of glaucoma, in addition to the pupillary-block type.
Do not worry about the size of the hole in your iris. Neither you nor your friends will notice it. It is usually placed in a portion of the iris which is covered by your upper eyelid. The size of the iridotomy is only that of a pin head.
Remember that the creation of a laser iridotomy is both safe and effective. There are a few risks. The purpose of an iridotomy is to preserve your vision, not to improve it.
